Beyond the Surface: Exploring Unconscious Bias in Pharmacy Practice

Pharmacy practice is a critical part of healthcare, where precision, objectivity, and attention to detail are paramount. However, even in this noble profession, unconscious biases can cast a shadow on patient care. In this post, we embark on a journey to explore biases in pharmacy practice and uncover how they impact patient outcomes.
What is unconscious bias?
Unconscious bias, also known as implicit bias, refers to attitudes or stereotypes that affect an individual’s understanding, actions, and decisions in an unconscious manner. Unconscious biases are often based on social stereotypes and can influence how people perceive and interact with others without their awareness. These biases can manifest in various forms, such as racial bias, gender bias, or age bias, and they can affect behavior, even when individuals consciously strive to be fair and impartial.
Types of unconscious bias:
There are over 150 diverse types of unconscious biases that fall into five broad categories based on which part of the brain is activated and our responses:
Similarity Bias: This bias can affect team dynamics and patient care. For instance, it may affect hiring practices, potentially leading to less diverse pharmacy teams.
Expedience Bias: Quick decision-making under limited information can influence medication recommendations or treatment plans, potentially affecting patient outcomes.
Experience Bias: Believing that everyone’s experiences are similar to our own may hinder understanding and empathy for patients with diverse backgrounds or health conditions.
Distance Bias: Valuing recent information more than past experiences can affect the assessment of a patient’s medical history or adherence to medications.
Safety Bias: Prioritizing perceived threats over rewards may affect patient provider relationships, potentially leading to misunderstandings or distrust.
For more types of unconscious biases and how to counteract, visit Ryerson University‘s “Equity, Diversity and Inclusion” document.
Technology and Bias:
In addition to unconscious biases, technology also plays a role in healthcare and pharmacy practice, influencing bias and patient care:
Tech Bias: Digital systems, like electronic health records and decision support systems, can perpetuate existing biases if not culturally competent.
Algorithm Bias: Healthcare tech algorithms may incorporate biases from historical data, affecting diagnosis and treatment recommendations.
Access Challenges: Patients lacking reliable digital access face barriers to medication information and healthcare instructions.
Digital Literacy: Patient digital literacy affects effective use of healthcare technology, requiring provider support.
Telehealth Impact: Expanding telehealth can create disparities for patients without reliable internet or devices.
Privacy Concerns: Worries about digital health information confidentiality affect patient engagement with tech-driven healthcare.
Human-Tech Interaction: Over reliance on automation can lead to overlooking patient-specific factors.
Economic Impact: The cost of healthcare tech implementation can affect medication and service accessibility.
Source of Truth
A “source of truth” refers to a trusted and authoritative reference or system that serves as the ultimate and most reliable source for verifying and confirming critical information related to patient care, medications, or treatment plans. This source is considered highly accurate and is relied upon to ensure the safety and quality of patient care.
In pharmacy practice, a “source of truth” can include official medication databases, clinical guidelines, electronic health records (EHRs), or other authoritative references that provide accurate and up-to-date information about medications, dosages, interactions, and patient histories. Pharmacists and healthcare providers use these sources to make informed decisions and to verify the accuracy of information before dispensing medications or providing healthcare services to patients.
The Swiss Cheese Model and Bias:
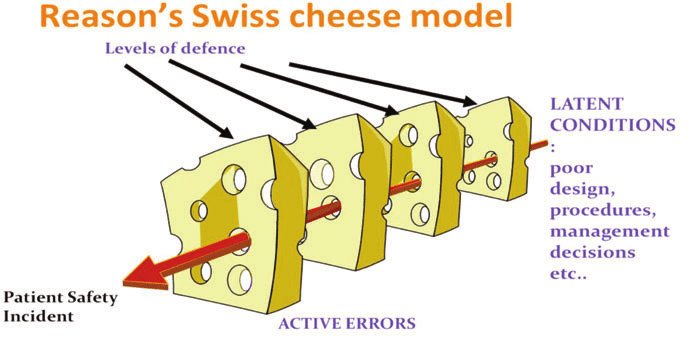
The Swiss Cheese Model, often used in healthcare to illustrate how multiple layers of defense can fail and lead to errors, is a relevant framework for understanding bias in pharmacy.
“Though computers certainly can be a solution to many kinds of medical mistakes, they can also be the cause (The Digital Doctor: Hope, Hype and Harm at the Dawn of Medicine’s Computer Age by Robert Wachter. McGraw-Hill 2015).” Statistics from a Harvard study found that 6% of errors were related to problems with computerized prescribing. We cannot over trust technology; we must balance trust in the program and on human review. Thus, we need to do reasonableness checks on every prescription.
When we think of the Reason’s Swiss cheese model of errors (see diagram below), our goal in terms of safety is to prevent the holes in the cheese from lining up. A source of truth check is far more effective in supplying a protective layer than trying to remove human error completely.
 https://phvfit.com/system-factors-in-patient-safety/
https://phvfit.com/system-factors-in-patient-safety/
Prescription Mix-Up: A Tale of Unconscious Bias
In a bustling pharmacy, Dr. Smith called with a crucial medication order for
Patient X. Alex, the diligent pharmacist, acknowledged the importance of the prescribed drug.
However, amidst a hectic day of filling prescriptions, the lines between medications blurred. Rushed and overwhelmed, Alex faced a challenging moment. Despite knowing the risks of confirmation bias, there was little time for double checking.
When it came time to assemble Dr. Smith’s order, an unconscious bias slipped through. The overwhelming familiarity with another drug, one often handled, influenced the choice. In that rushed instance, it seemed like the “correct” medication, even though it deviated from Dr. Smith’s prescription.
This incident serves as a stark reminder of how biases, even when acknowledged, can subtly impact decisions. In the precision-driven world of pharmacy practice, these biases can have profound implications for patient care.
Steps to Overcoming Unconscious Bias:
- Acknowledge Your Biases: Recognize your biases.
- Self-Examination: Reflect on triggers and influences.
- Bias Mitigation Strategies:
- Self-Reflect: Understand life experiences’ impact.
- Learn About Others: Respect diverse perspectives.
- Observe and Reflect: Pay attention to bias challenges.
- Promote Inclusion: Practice active listening.
Unconscious biases can be changed and slowly unlearned. We can start becoming aware of our own unconscious biases through the Implicit Association Test (IAT) developed by Harvard University.
Conclusion:
In the realm of pharmacy practice, addressing bias is not just an option; it is a moral and professional obligation. Our journey explored the intricacies of biases in human interactions and technology’s influence. Let us illuminate the path to equitable healthcare, one layer at a time, for a fairer and more effective system.
About the author;
Devaki Grenier is a passionate Pharmacy Technician, dedicated to helping patients and ensuring their well-being through more than 12 years of experience in the field.

3 replies on “Beyond the Surface: Exploring Unconscious Bias in Pharmacy Practice”
Oh this was very interesting, I really liked the swiss cheese reference too it really helps to put it into perspective! I will definitely be referring back to this blog from time to time for reminders!
Thank you! Your comments and opinions are valuable to us! What would you like to hear about in the future?
Thank you! Your comments and opinions are valuable to us! What would you like to hear about in the future?